Customer Journey: The Eye Examination
Usually, a person will have their eyes tested when they feel that the ‘vision doesn’t seem quite right’. As soon as any visual symptoms arise it is advisable to book in with your local opticians to address the issue. In the majority of cases, a pair of spectacles will enhance the patient’s vision and bring them to the optimum level of correction to best cater to the visual anomaly.
Image (1) Credit: Shutterstock
But, what if the vision is clear and ‘perfect’? Would you consider having your eyes tested for any other reason? The answer should be, yes. Everyone should have their eyes checked regularly. The Association of Optometrists (AOP) recommend an eye exam should be every 2 years, or as advised by your Optometrist1. There are several reasons for this. Let us explore why.
“Why should I have an eye exam?”
1. Vision test:
The 1st reason that would come to mind is to simply check the actual vision. Is a patient straining to see in the distance? This would have implications for daily tasks such as driving, looking at a bus number or even ‘keeping an eye’ on the kids playing in the garden. Alternatively, is a person straining to read books or look at their computer? If so, this would suggest a possible prescription for ‘near vision’. The topic of ‘visual correction’ is wide and varied but the good news is that spectacles and contact lenses can correct a multitude of eye prescriptions.

Image (2) Credit: Shutterstock
2. The health of the eye:
The eyeball is a complex organ consisting of various layers and structures to manage one of our most important senses; vision. The routine eye exam will assess the working order of all of these structures from the front of the eye, to the back.
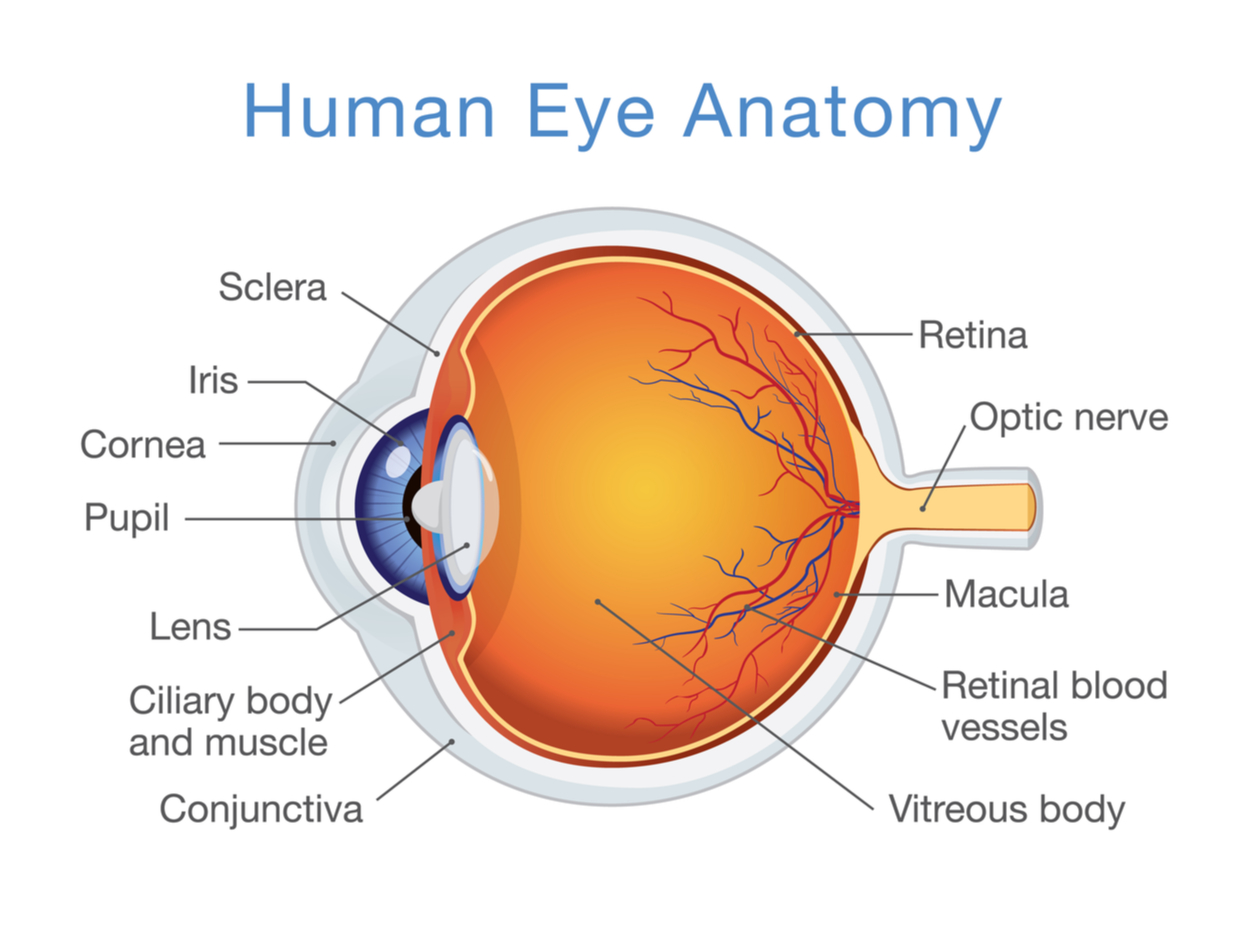
Image (3) Credit: Shutterstock
As an example, one such structure is the Lens of the eye (the Crystalline lens). This lens should be transparent to allow light to enter the eye and focus on the retina at the back of the eyeball. If the crystalline lens becomes cloudy (due to UV damage, ageing or medicines), this is referred to as a cataract. Cataracts are the most common cause of vision loss in people over the age of 40 and therefore it is a vital reason to regularly have one’s eyes tested2.
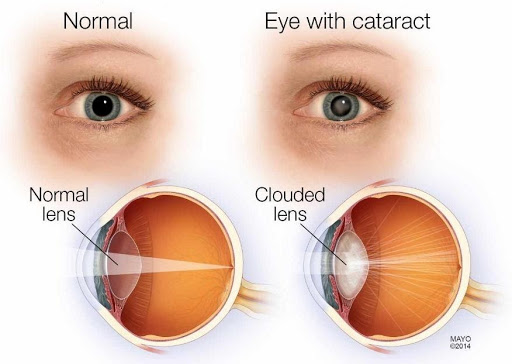
Image (4) Credit: Mayo Clinic
3. The health of the body:
Most people would have heard that “the eyes are the window to the soul” and therefore, as your optician assesses your eyes, they get a glimpse into your entire body’s health as well. The main observations that can be made are as follows3.
a. Diabetes – observations include ‘leaky’ blood vessels that may bleed in the eye or the observation of ‘cotton wool’ spots on the retinal surface.
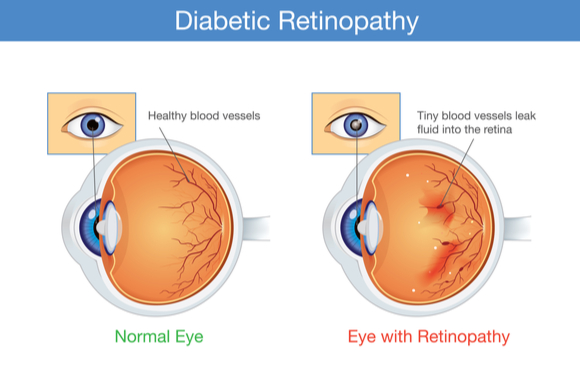
Image (5) credit: Medical News Today
b. Hypertension – the blood vessels at the back of the eye may appear more ‘bendy’ and arcuous than a healthy eye. This can indicate high blood pressure.
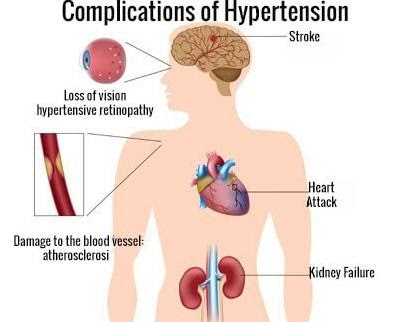
Image (6) Credit of hypertension.ucoz.net
c. Autoimmune diseases – inflammation of the eyes and other ocular signs could be indicative of autoimmune diseases such as Lupus.
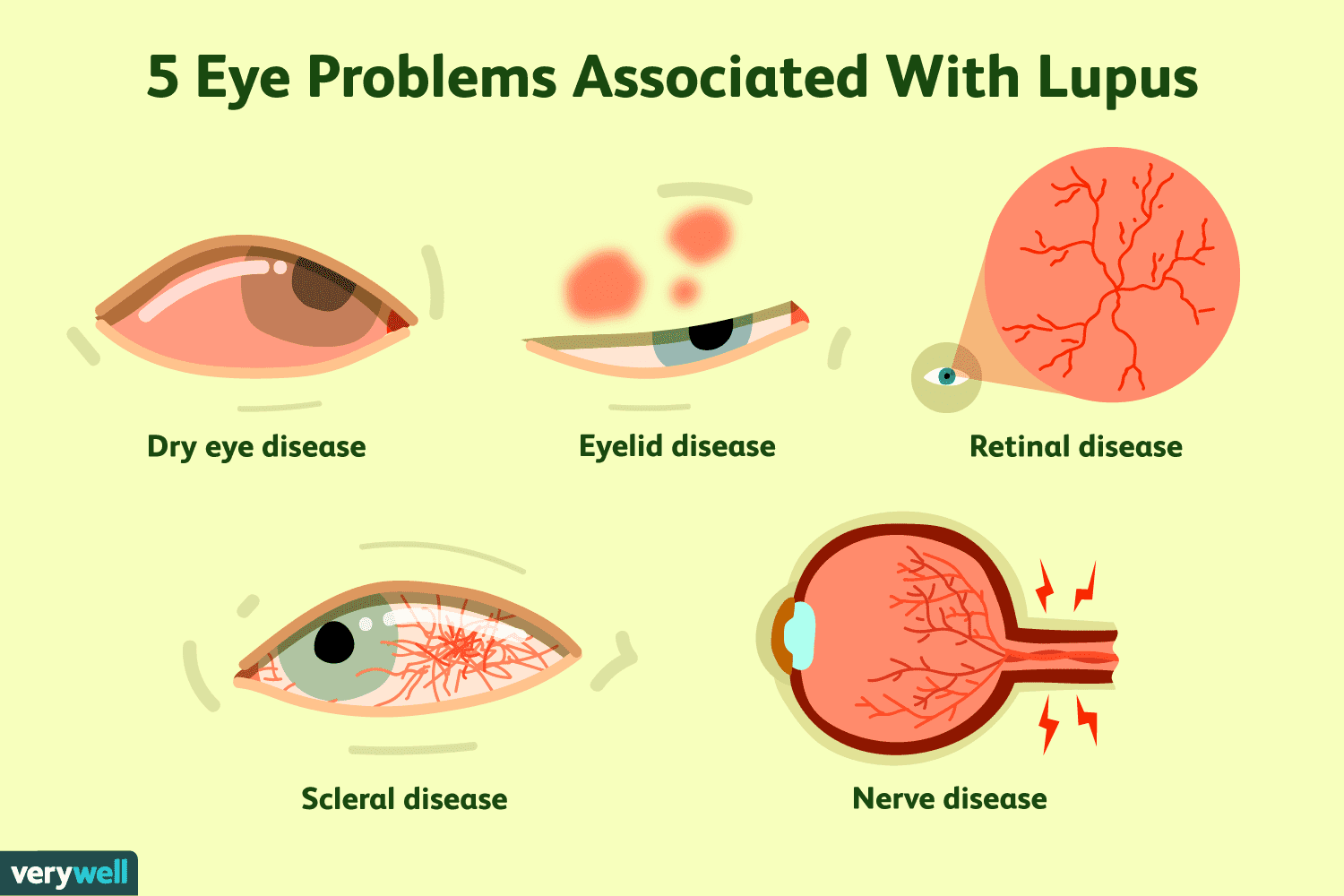
Image (7) Credit of Very-well health
d. High cholesterol – Some customers are advised to see their GP for a cholesterol check after the eye exam. This would be because the optician would have observed signs such as a whitish ring around the cornea (arcus senilis). The blood vessels of the retina may also be indicative of increased cholesterol levels.
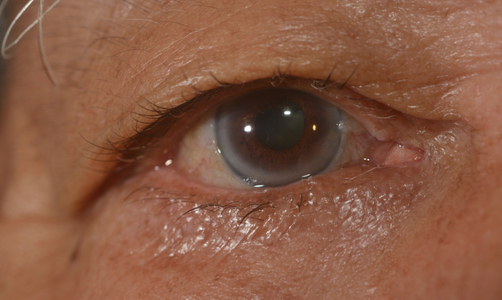
Image (8) credit: Arcus Senilis: Shutterstock
e. Thyroid disease – protruding eyeballs are a possible sign of thyroid disease. Once again, the optician may request that a patient have a blood test to evaluate the thyroid function.
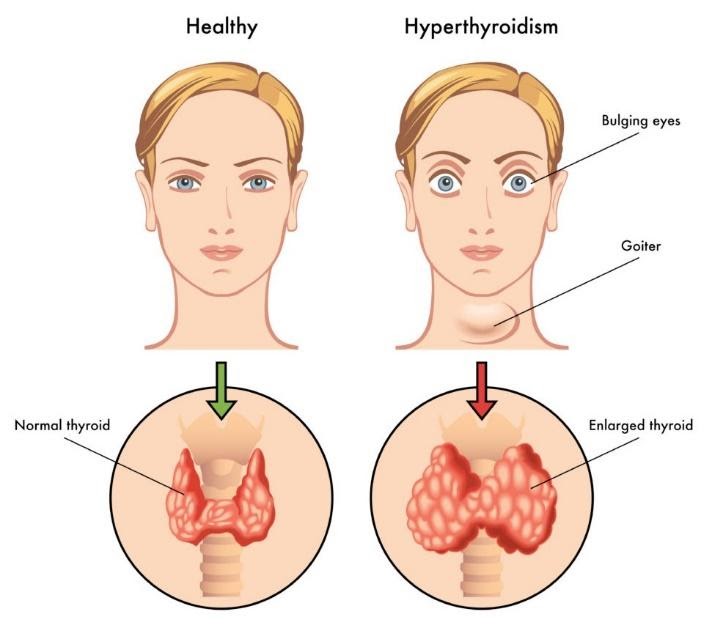
Image (9) Credit: Newton Medical Center
f. Cancer or Tumours – Routine eye exams require observations to be made of the entire eye socket, the surrounding skin as well as intraocular observations. Unusual pupil sizes between both eye’s, skin lesions, ‘field visual loss’, abnormal eye movements and swelling of the optic nerve (image 10) can indicate the possibility of cancer or tumour.
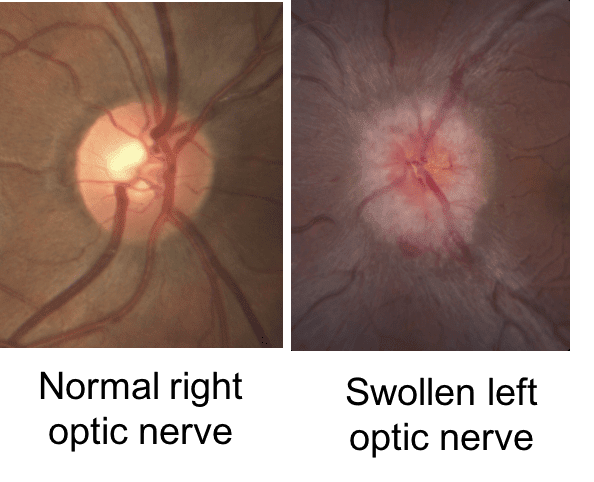
Image (10) courtesy of Neuro-Ophthalmology – Swollen left optic nerve due to elevated pressure around the brain
4. Peripheral viewing ability:
A comprehensive sight test must include a ‘field visual assessment’. The sight test will record a patient’s subjective response when viewing a test room chart and this records the viewing ability in the central vision. But peripheral vision is also vitally important because it is your peripheral vision that allows you to detect an oncoming object before it is in your clear sight of vision. Hence, if your field visual plot gives a 100% positive result, your optician can be satisfied that as a patient, you can see any possible hazard approaching you from the side. The field visual test is an integral part of holding a valid DVLA licence4.

Image (11) Credit: Fleet Point – Poor peripheral vision due to Glaucoma
5. Post-trauma:
If someone has been in any type of accident causing head injury (car accident or a fall), it is wise to include an eye exam as part of any post-trauma aftercare. Eye and vision problems can be quite common after a brain injury5.
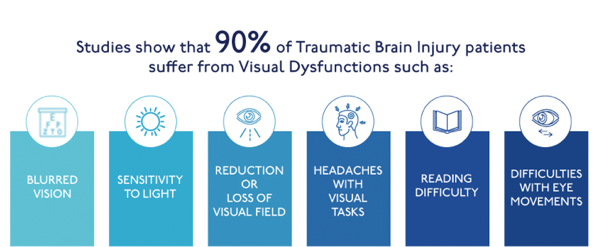
Image (12) Credit: noravisionrehab.org
6. Children & learning:
Good sight is linked to learning6. By testing children’s eyes, parents can manage any visual problems at an early onset. If children are struggling to see projector screens, black/whiteboards or even struggling at near sight, this can have adverse effects on their learning abilities.
Image (13) Credit: Shutterstock
What to expect at your Eye Test?
History & Symptoms: The practitioner will ask routine questions during the eye exam. For example, “What is the reason for the visit today?”. From this, the optician can gauge if the patient has any visual or health concerns. Other questions will explore the patient’s general health, medical history, including a list of medications, family health, occupation, lifestyle & hobbies.

Image (14) Credit: nhrmc.org
This information will give the practitioner vital clues about how to best manage any issues that may arise. Also, by exploring a patient’s symptoms and delving into family history (heart disease, diabetes, glaucoma, high blood pressure), the optician will be alerted to future conditions that could possibly manifest. Coupled with the results of the remaining sight test, the optician can diagnose and formulate the best course of action, where required.
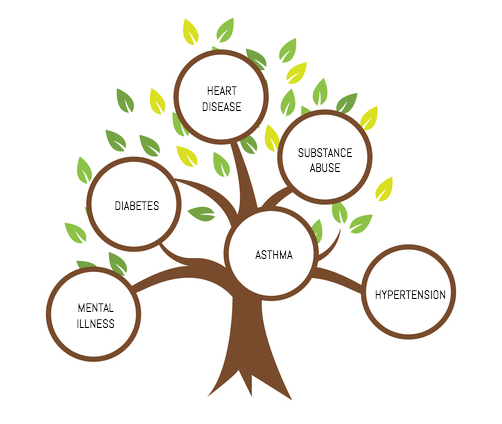
Image (15) Credit: Shutterstock. Edited by Oodo
The Clinical Tests: The clinical assessment is best described in all of its stages. They will be broken down as follows.
- External examination of the eye
- Internal examination of the eye
- Refraction (Is a prescription required for correction?).
External Examination:
- Pupil Reactions: Pupil reflexes are often checked in Hospitals, post-trauma, so the relevance of this test is important. The pupil will constrict and dilate naturally according to the amount of light exposure. In bright lighting, the pupils will be smaller by the action of constriction and conversely, in dim lighting, the pupils will dilate to allow as much light into the eye as possible, to enhance the vision. The optician will sweep a pen torch over the eyes to check that the pupils are reacting correctly and consensually, whereby, the response in 1 eye is mimicked by the other eye also. Poor pupil reactions could be indicative of optic nerve damage or disease. A non-responsive pupil or an odd-shaped pupil could indicate Iritis (or anterior Uveitis) which is the inflammation of the iris causing pain and light sensitivity. Therefore, odd pupil sizes and abnormal responses would need to be investigated further.
Image (16) Credit: Socratic.org – light intensity
- Ocular Motility: This term refers to the movement of the eye muscles and in consequence, the movement of the eyeball in all positions of gaze. The optician will want to see the equal alignment of both eyes and consensual movement. A deviation from the norm may be observed as an obvious ‘squint’ (strabismus) where both eyes appear to be looking in different directions. This would indicate that the extraocular muscles are not working in unison. In children, the cause could be a visual problem7. In adults, the cause may be due to trauma, weakness of eye muscles, surgery or tumors8. Treatments include spectacle correction, eye exercises or surgery.
Image (17) Credit: Shutterstock
- Stereopsis (Depth Perception): Depth perception is the ability of both eyes to fuse an image, in the brain, and to see it in its 3-dimensional form. It is developed from an early onset in life, at approximately 3 months of age9. It allows us to gauge how far something is from us and how quickly it is approaching10. Causes of reduced stereopsis include poor vision, a ‘lazy eye’ (where one eye is weaker than the other), squints and ocular traumas. A common stereo acuity test is the ‘Titmus Stereo Fly Test’ (image 18). The test is designed to suit children as well as adults. Wearing the polarised 3D viewing spectacles, the patient looks at the various pictures, with both eyes, and describes how they perceive the images. With the optimum fusion between both eyes, the images should appear to ‘stand out’ in their 3D form. Where the images appear flat and without form, it would suggest interference in the patient’s stereopsis.
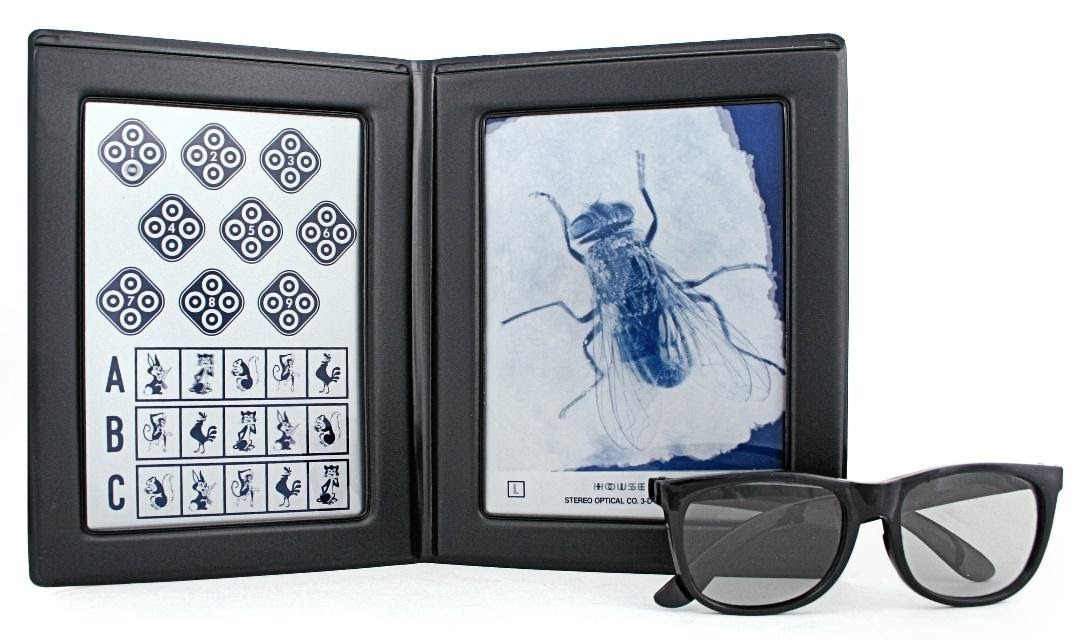
Image (18) Credit: Stereo Optical
- Colour Perception: A widely used test for colour perception is the ‘Ishihara Test’ (image 19). By viewing numbers hidden in a mosaic style plate, presented in various colours and backgrounds, it is the most comprehensive colour perception test to date.
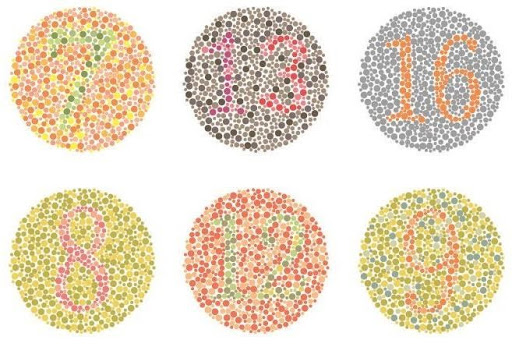
Image (19) Credit: All About Vision – The Ishihara Test
Colour vision is vital sensory information for our day-to-day tasks. We are able to discriminate between objects, characteristics, our environment and the location of something just by its border or shadow11. Photoreceptors in the retina respond to light, enhancing our ability to differentiate the colour spectrum. If the retinal photopigments are compromised, the ability to see with definition is impaired, making colour recognition inaccurate. Colour blindness is a genetic condition whereby the retinal cells are abnormal. However, other factors can contribute to the lack-lustre of colour which includes damage to the optic nerve12, cataracts and AMD (age-related macular degeneration).
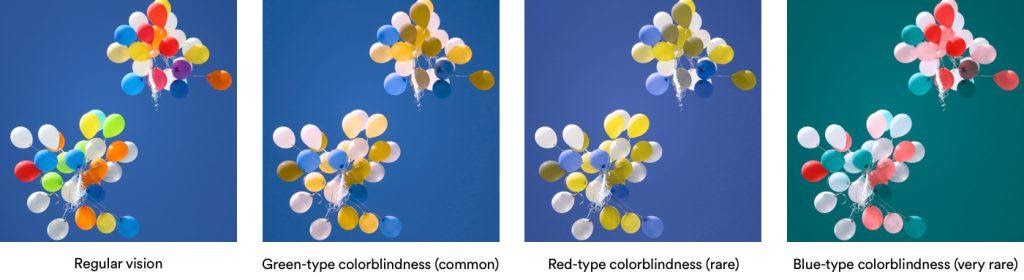
Image (20) Credit: 22 Create – colour blindness & design
- Slit Lamp Observations: The slit-lamp, or biomicroscope, is a binocular microscope that allows the optician to view external and internal eye features under various light sources and magnifying powers. The patient will be asked to sit close to the instrument with their chin resting on the chin rest and their forehead against the top bar. The optician will fine-tune the alignment of the binocular setting to coincide with the position of the patient’s eyes. The aim is to ensure a comfortable and constant posture during the course of the test. If the patient moves their head or chin away from the desired position, it alters the viewing capacity and hinders the examination.
Image (21) credit: Medical News Today
Observations of the eye start with the most external features first, gradually increasing the magnification to view through the various media of the eye layers. Areas of observation include the eyelids, cornea, sclera, the tear-film, iris and the crystalline lens. With the aid of an extra magnifier (the Volk lens), the observer can view the retina and optic nerve. The Slit Lamp is an intrinsic tool in detecting ocular anomalies such as corneal lesions, dry eyes, blepharitis, cataracts, irregular pupils, detached retina13, diabetic retinopathy and optic nerve changes.

Image (22) Credit: Optician Online – Slit Lamp observation of the Optic Nerve
Internal Examination:
- Field of View Test: As mentioned earlier, it is important to assess a patient’s peripheral vision to determine that the patients ‘side vision’ is functioning just as well as the central vision. A ‘visual field test’ measures the performance of the eye in the central and peripheral zones. Some ‘field of view’ loss can go unnoticed by the patient14 which is why it is necessary to conduct this test as part of the eye exam.
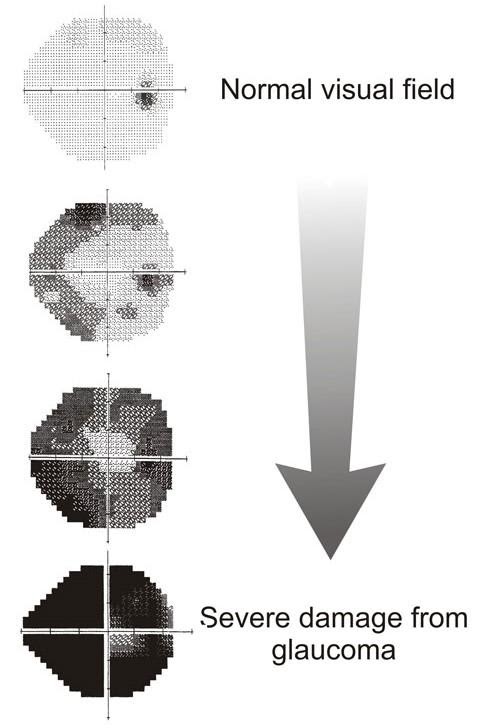
Image (23) Credit: glaucoma.org.il – Visual field damage in glaucoma
Everyone has a natural ‘blind spot’ where the optic nerve connects to the back of the eye, but any unusual blind spots could be indicative of more serious conditions. Some of these conditions include glaucoma, retinal disease, optic nerve damage, brain tumours and stroke. The most widely used devices to measure the ‘field of view’ are automated instruments whereby the patient fixates their vision upon a target and responds to the stimuli presented to them.
Image (24) Credit: Verywell health
- Tonometry (Eye Pressure): There are a variety of Tonometers on the market. Some touch the surface of the eye, and others are non-contact devices that blow a puff of air at the eye. The aim is to measure the pressure within the eyeball (the IOP – Intraocular pressure). The procedure is very quick and painless. It is normal to take a few readings and to score the mean result.

Image (25) Tonometer. Credit: Shutterstock
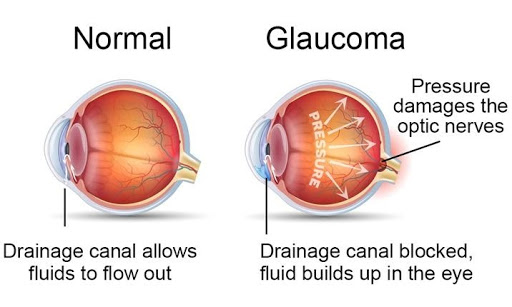
Image (26) credit: Mount Elizabeth Hospital, Singapore
The pressures can vary from morning to night and can fluctuate with stress levels. However, unusual oddities, away from the norm, can be signs of ocular pathology. Unusually different pressures between both eyes or elevated pressures may be indicative of Glaucoma. An increase in pressure, in the eyeball, will press against the optic nerve and cause damage.
Coupled with anomalies in the ‘field visual test’, this would most certainly suggest Glaucoma. A patient may be asymptomatic of any pathology, so measuring the pressure is very important. Since Glaucoma is genetic, any ‘family history’ of glaucoma should be mentioned at the sight test.
- Ophthalmoscopy: The optician will use an ophthalmoscope to view the deeper layers of the eye. This instrument is a handheld device, much like a torch with variations in viewing settings. Observations are recorded of the fluid of the eye (the vitreous humor), the retina, blood vessels and the optic nerve head. This is the most traditional viewing method to see the back of the eye and to check for signs of glaucoma or retinal abnormalities. The practitioner has to come in closer to the patient’s eye when viewing through the ophthalmoscope whereas, with the slit-lamp and volk lens, some distance can be maintained. The observer will ask the patient to look in different positions of gaze, to assess as much of the back of the eye as possible.

Image (27) courtesy of specialty.mims.com, Malaysia – Ophthalmoscopy
- Retinal Scans: With advancements in technology, it is possible to view larger areas of the back of the eye using high-magnification photographs, and recording these observations as digital images stored against the patient’s medical record. Image 28 shows a partial retinal observation when viewed through an ophthalmoscope. Image 29 is of a healthy eye (right eye), highlighting a wider field of view when observed through a retinal scanning machine. This image shows the optic nerve zone (the round, pale area in the image), the blood vessels and the macula (the denser coloured zone which is the vital ‘seeing’ part of the retina). Traditional methods of observing the retina are restricted by the smaller view-finder of the ophthalmoscope or slit lamp. Devices that are designed to take retinal pictures are an excellent tool to record exact observations. These records are stored and can be used for comparisons for future sight tests (monitoring changes) and can be forwarded to specialist consultants for referrals, where further investigation may be required.
Image (28) Credit: Yang-low.com Partial Retinal View with Ophthalmoscope
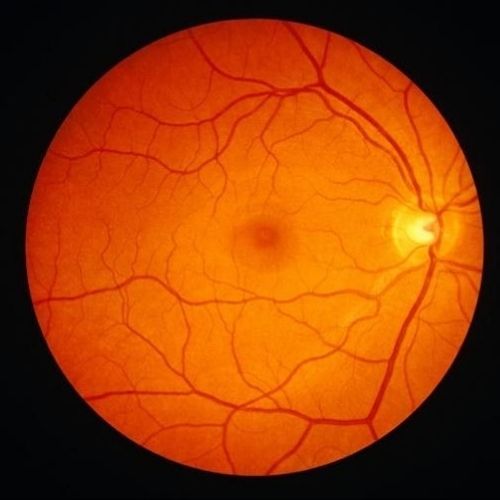
Image (29) Credit: verywellhealth.com – Digital Retinal Imaging
- OCT (Optical Coherence Tomography): OCT devices progress retinal photography to the next level of development. As well as taking retinal photographs, the OCT machine uses light-wave technology to take 3D images through cross-sections of the retina15. Whilst 2D photos clearly highlight surface anomalies, the 3D images allow observations to be detected at a foundation level. Early signs of macula disease, diabetic retinopathy and glaucoma can be detected before they manifest at the surface level. The vital layers of the retina and the optic nerve zone can be viewed, measured and monitored for continuous eye health.

Image (30)Credit: provision.com.au – OCT machine
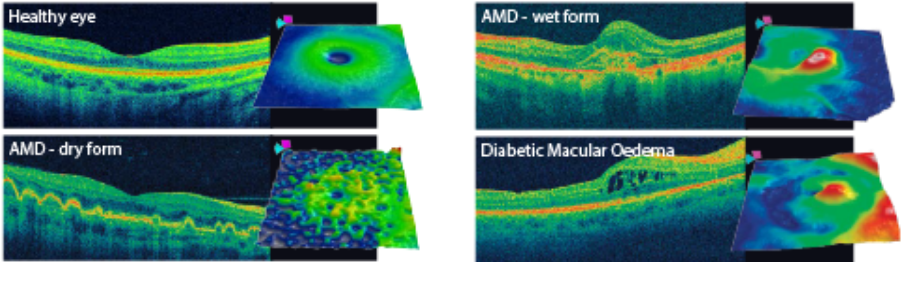
Image (31) from Bromley Eye Centre – OCT scans
Refraction:
- Autorefractor: State-of-the-art autorefractors, are machines that give a fairly accurate estimate of a patient’s prescription. The patient is seated at the computerised autorefractor and asked to view a target in the instrument. This image will come in and out of focus whilst the autorefractor measures how light enters the eye and is reflected at the retina. When light does not focus on the retina accurately, we refer to this as refractive error. The autorefractor measures this error and determines the proximate correction required to be prescribed in spectacles or contact lenses. The test is very quick and easy. It especially helps where patients cannot give the best subjective responses, such as children or those that have communication difficulties.

Image (32) credit: Lunea Technology, USA – Autorefractor

Image (33) credit: Praxisdienst.com – Retinoscope
- Retinoscopy: The retinoscope is a handheld device, not too dissimilar to the ophthalmoscope. However, the retinoscope was designed to observe the light reflex from the retina to objectively measure the refractive error from the patient’s eye. Hence, this piece of equipment is the traditional technique to estimate a patient’s prescription. Just like the automated autorefractor, a retinoscope is a valuable tool for estimating the prescription for non-verbal patients.
- The Test Chart: To test the vision, the practitioner will be guided by the results from the retinoscopy or autorefractor and use this as a start point to fine-tune the prescription. With the patient sat down, their vision is measured using a Snellen chart, named after its creator in the 1860s16. In the UK, we measure the optimum vision in metres and in the US, vision is measured in feet. The patient will have 1 eye covered whilst the other eye is being measured on the Snellen chart. The vision is tested as the patient reads out the letters from the top of the chart, downwards, where the letters become progressively smaller. The ideal vision to be attained would be 6/6 vision (measured in metre’s), or 20/20 vision (measured in feet). This means that the patient can see something at 6 metres (or 20 feet), what a person with good vision can see at the same distance.
Image (34): Snellen Eye Chart
To correct and balance the prescription is referred to as ‘refraction’. The optician will test the sharpness of the vision using a series of lenses that correct long-sightedness, short-sightedness and astigmatism. ‘Vision’ refers to the patient’s ability to see on the test chart without any correction in place, whilst the ‘visual acuity’ is the vision measured with the prescription in place. The optician may use a trial frame with interchangeable lenses or a phoropter head, which is placed close to the patient’s eyes and the lenses can be changed manually or through an automated system. Likewise, to test the vision for reading, a similar handheld chart is used to measure the uncorrected vision, followed by, the refraction for the amount of correction required to give the desired acuity.

Image (35) Credit: Digital Phoropter: Shutterstock
Other tests & check-ups:
Dilation drops: Some customers are required to have dilation drops to be instilled at their eye exam. This is to widen the pupil aperture so that the optician can get a larger field of view for the back of the eye. The drops take approximately 20-30 minutes to achieve the desired effect. Once dilated, vision is momentarily impaired especially at the near focus. This can last for a few hours. The eyes will be particularly sensitive to bright light since the pupils are artificially kept open and inert to the natural response to constrict in the brightness. Therefore, the patient is advised to bring sunglasses to wear after the sight test and to make suitable arrangements for their journey home.
Image (36) courtesy of American vision at the court
Contact-Lens assessments: A separate appointment is required for contact-lens related check-ups. The fitting and continued aftercare of contact lenses must be monitored on a regular basis. Essentially, the contact lens is a foreign body introduced to the eye (for refractive or cosmetic use). Therefore, these assessments are required more frequently than a sight test to ensure that the contact lenses are not causing any adverse reactions to the eye and its natural function. Where a sight test reviews the entire functionality of the eye, the contact-lens appointment reviews the fitting of the contact-lens and its effect when in situ. Patients are required to wear their contact lenses to the appointment (unless it is the initial fitting appointment) and bring their spectacles to the appointment.
Image (37) Credit: Shutterstock
“Do I need to do anything to prepare for my Sight Test?”
To prepare for your sight test, here is a list of things that you can do to help the process:
- Attend the appointment at the stipulated time slot.
- Allow enough time for the examination, especially if additional screening is required (retinal scans, OCT).
- Bring any current spectacles, contact lenses and the CL packaging.
- If you have the last prescription from elsewhere, please bring that with you
- A list of medications taken over the last 6 months to current time
- Bring hospital letters pertaining to the eye and ocular history/surgery
- Sunglasses (prescription or non-prescription): To be worn home after a dilation appointment.
- Manage transportation home if you cannot drive after a dilation
- Bring a language interpreter to avoid miscommunication
- Avoid heavy eye make-up

Image (38) courtesy of freepik.com
And, to round things off…Sight Test Room Etiquette:
- Switch off your phone or turn it to silent mode (your optician doesn’t take calls during ‘your’ eye exam so please refrain from doing this).
- Avoid food or drink in clinical places.
- Avoid distractions in the room – please make arrangements for child or pet care. Distractions delay valuable clinic time but also increase the margin for error whilst testing.
- When children are in the room or being tested, please inform them not to touch any equipment.
- Be concise – please answer the questions being asked as clearly as possible without digressing.
- DO NOT SPREAD GERMS: If you are unwell, please phone and cancel your appointment.

Image (39) Credit: Association of Optometrists
Continue the Customer Journey with: The Opticians – Part 2 – Buying Spectacles
Article Author: Ms Reena Bains (BSc) Hons FBDO
Article Editor: Mrs Meena Puar MCOptom FBCLA
-
Aop.org.uk – NHS sight test eligibility
-
Reference from allaboutvision.com
-
Yoursightmatters.com
-
Gov.uk – Guidance – Visual disorders assessing fitness to drive
-
Everydayhealth.com, 20.01.2009
-
C4sightcare.com
-
NHS.uk – Conditions, Squint
-
Shalby.org – Squint: Causes, Symptoms & Treatment.
-
IOVS.arvojournals.org – The critical period for susceptibility of human stereopsis
-
Courses.lumenlearning.com – Advanced topics in perception
-
Scholarpedia.org – Color Vision
-
Webmd.com -What is color blindness?
-
Bryantso.com – eye exams
-
AAO.org – eye health – Eye exam & vision testing basics
-
AAO.org – eye health – What is an OCT?
-
AAO.org – eye health – Eye chart
Posts by Oodo may include affiliate links. This means that we make a small commission from referrals and purchases at no extra cost to you. Thank you for your kind support.








